Ductus Venosus
Ductus Venosus Definition
Ductus venosus Arantii (after Giulio Cezare Aranzi) is an anatomical structure, a vascular canal, which is only present in the fetal development, facilitating fetal circulation. It connects the umbilical vein and vena cava inferior (VCI) and is significant because it represents a shunt to lead the blood away from the liver of the fetus to the heart.
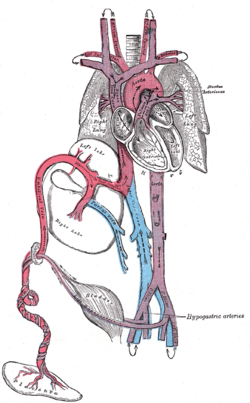
Figure 1 Fetal anatomy of the inner organs. (1)
Embryology & Functions
Ductus venosus (DV) is a temporary canal which obliterates after birth, beginning as of a couple of days after birth, and is finished when the baby is approximately 1-3 months old. Ductus venosus is a cone like canal with narrowed part which connects with the umbilical vein, and the wider which releases blood into the vena cava inferior.
The majority of blood enters the ductus venosus even though there is another way, through port vein to the VCI. The blood enters the DV with great velocity and under great pressure because of the narrowed part and brings the oxygenated blood from umbilical vein to the heart.
However, the blood from DV can enter either VCI directly or the right atrium and left atrium, and this blood then goes to the aorta. This system with shunt enables the liver to be bypassed, and the blood to be redirected from it, because it is not yet fully formed and developed.
The fetal liver doesn’t need that much oxygenated blood, and the sufficient amount of blood is provided with portal vein. The same principle is allowed with ductus arteriosus, which bypasses the lungs, in order for oxygenated blood to spread to the whole fetal body more quickly. (1) (2)
The blood that enters the heart is actually mixed: oxygenated from the umbilical vein and placenta with deoxygenated blood from the VCI. This partially deoxygenated blood spreads through the whole organism.

Figure 2 Blood travel from the placenta, umbilical vein and to the ductus venosus and Vci and to the heart. The blood becomes partially deoxygenated (4)
Abnormalities
Ductus venosus persistens – Patent DV
If the ductus doesn’t obliterate and transform into a thin fibrous ligament, which normally happens after birth, the blood continues to flow through the DV, bypassing the liver. This is more frequent occurrence in premature babies.
There is a possibility that the prostaglandins which are responsible for keeping the ducts open during fetal life to continue to be increased, thus unabling the ductus to close.

Figure 3 Persistant ductus venosus is shown with red arrow (2)
Absent DV – Agenesis of DV
It is a rare abnormality with which a fetus can survive. When there is no DV, blood flows through the liver or outside the liver with some adjuvant shunts to allow the drainage. This abnormality is often associated with some genetic disorders and malformations of other organs. The shunts that form instead of DV are either extrahepatic or intrahepatic. Extrahepatic shunts bypass the liver. This way, umbilical vein is connected to the iliac vein, or to other veins : the IVC, renal vein, or right atrium or very rarely left atrium. Intrahepatic shunt means that the umbilical vein is connected to a portal sinus in the liver. (3)
Symptoms
Symptoms depend on the abnormality of the DV. If the DV is still present after 1-3 months, overfilling of the veins in the liver with liver symptoms, hepatomegaly with portal hypertension, jaundice and hyperbilirubinemia, following the hepatic atrophy and inability to thrive would appear, but usually asymptomatic for some time or many years, unless there are other abnormalities of the heart. In that case a child will experience cyanosis and hypoxia.
When the liver vein system is filled with blood, that blood transudes into the peritoneum and surrounding tissue via diffusion, and this way a baby may develop generalised edema (hydrops), ascites and hepato-pulmonary syndrome. Eventually, the baby’s heart enlarges (cardiomegaly).
Diagnosis
The atresia (absence) of the DV can be noticed antenatally via ultrasound and Doppler sonography. Abnormal circulation and development of only one umbilical artery and consequences of the overload, cardiomegaly and hydrops. A gynaecologist/obstetrician will follow the blood flow and check for alternative shunts that activated instead of DV. Patent DV is suspected after clinical exam and thorough history from the mother, but also with genetic testing and karyotyping and confirmed with ultrasound with echocardiography, CT or CECT.
Treatment
Patent DV is best treated with surgical procedures: balloon occlusion (as a test before the operation, to check what consequences would the closure bring), ligation or banding. They showed good outcomes and reduction of symptoms. The procedures can be performed as minimally invasive surgeries, percutaneously. Other options for treatment include liver transplantation and trans-catheterisation. Some studies support the theory that DV shouldn’t be closed too early, because of the possible late spontaneous closure. (4)
Absent DV treatment depends on the severity of symptoms and the level of oxygenation to the tissue via shunts. If the drainage satisfies the drainage and enables proper blood flow surgery isn’t necessary, Many of the babies survive if there aren’t any abnormalities associated. If there are some heart abnormalities or signs and malformations that appeared as a consequence of aneuploidy have worse prognosis, and some of the babies die. (5)
Works Cited
- Ductus venosus. Wikipedia. [Online] [Cited: 2 16, 2017.] https://en.wikipedia.org/wiki/Ductus_venosus.
- Cardiovascular System – Ductus Venosus. UNSW Embriology. [Online] [Cited: 2 15, 2017.] https://embryology.med.unsw.edu.au/embryology/index.php/Cardiovascular_System_-_Ductus_Venosus.
- Regulation of blood flow through the ductus venosus. DI, Edelstone. 1980, J Dev Physiol.2(4), pp. 219-38.
- Fetal circulation. Radiology and Nuclear medicine. [Online] [Cited: 2 16, 2017.] https://tomography.wordpress.com/2007/11/24/solution-to-picture-of-the-week-8-and-this-weeks-image/.
- Absence of the ductus venosus. Sothinathan U, Pollina E, Huggon I, Patel S, Greenough A. 2006, Acta Paediatr 95(5), pp. 620-1.
- Percutaneous device closure of persistent ductus venosus presenting with hemoptysis. Subramanian V, Kavassery MK, Sivasubramonian S, Sasidharan B. 2013, Annals of Pediatric Cardiology 6(2), pp. 173-5.
- Patent ductus venosus presenting with cholestatic jaundice in an infant with successful trans-catheter closure using a vascular plug device. Chacko A, Kock C, Joshi JA, Mitchell L, Ahmad S. 2016, Indian J Radiol Imaging 26(3), pp. 377-82.
